The CHUMS Study: Cultural HUmility in Mental health Services
Co-Producing Actionable Knowledge to Strengthen Cultural Humility in Irish Mental Health Services
Background
Research shows that ethnic minority populations experience mental health challenges at disproportionately high rates and often face significant barriers in accessing appropriate mental healthcare. Human rights law and mental health policy emphasise that everyone has the right to have their mental healthcare needs met. While efforts to improve mental healthcare for ethnic minority populations have often involved training professionals in cultural competence, these programs, though effective in enhancing short-term knowledge and attitudes, have not led to sustained improvements in the mental health experiences of ethnic minority communities.
For this reason, cultural competency training alone is not enough. There is also a pressing need for cultural humility—a deeper, ongoing approach that encourages mental health services to examine and challenge the “standard” practices that contribute to unequal care experiences for ethnic minorities. Cultural humility goes beyond competence by asking us to critically reflect on how our ‘normal’ ways of thinking, acting, and organising care might impact diverse communities differently. However, as this is a newer concept, there is limited research on the specific actions it involves or how to implement and evaluate it effectively.
In answer to this gap in research knowledge, the overarching aim of The CHUMS study is to co-produce a model of cultural humility in mental healthcare, which is context responsive, implementable, and measurable.
The CHUMS Study’s co-produced model of cultural humility in mental healthcare will be achieved through four interrelated Work Packages (WPs):
WP1
Community Based Participatory Research
WP1 is The CHUMS Study’s ‘Together’ phase. In this WP, we aim to conduct Community Based Participatory Research (CBPR) in which knowledge end users are genuine collaborators in the design, conduct, and dissemination of The CHUMS Study. We will be monitoring and evaluating our conduct of CBPR over the lifetime of The CHUMS Study to capture best practices and lessons learned as we strive to achieve meaningful co-production within and co-ownership of The CHUMS Study between all academic, community and lived expertise team members.
WP2
Mapping the Implementation Climate
WP2 is The CHUMS Study’s ‘Understanding’ phase. In this WP, we aim to assess the capacity and receptivity currently within Ireland’s mental health services to integrate cultural humility in mental health services. We will ask research questions such as: Are mental health services and practitioners currently competent in cultural humility? What do they need to help strengthen their competency in cultural humility? What factors enable or hinder the implementation of culturally humility in Irish mental health services?
WP3
Envisioning a ‘Culturally Humble Model of Mental Health Care’
WP3 is The CHUMS Study’s ‘Design’ phase. In this WP, we aim to co-design a model of culturally humble mental healthcare. We will ask research questions such as: What should a culturally humble model of mental health care look and feel like? What should be the essential and desirable components? What are the quality indicators of a culturally humble model of mental healthcare and how will we measure them?
WP4
Creating Strategic Implementation Guidance
WP4 is The CHUMS Study’s ‘Design’ phase. In this WP, we aim to create tailored strategic implementation guidance in support of strengthening cultural humility in mental health. We will ask research questions such as: What implementation strategies do we need to support the effective implementation of a culturally humble model of mental healthcare? How best can we tailor our implementation strategies to ensure they are context-responsive, acceptable and feasible in practice.
Our Approach
The CHUMS Study draws on the principles of Community-Based Participatory Research (CBPR), a method rooted in a deep respect for diverse knowledge systems, or “multiple ways of knowing.” CBPR emphasises collaborative, equitable partnerships among researchers, stakeholders, and community members throughout every phase of the research process—from formulating questions to sharing findings. By enhancing the “3 R’s” of research—rigour, relevance, and reach—CBPR is uniquely positioned to bridge the gap between research and practice, creating pathways for impactful change in mental health care.
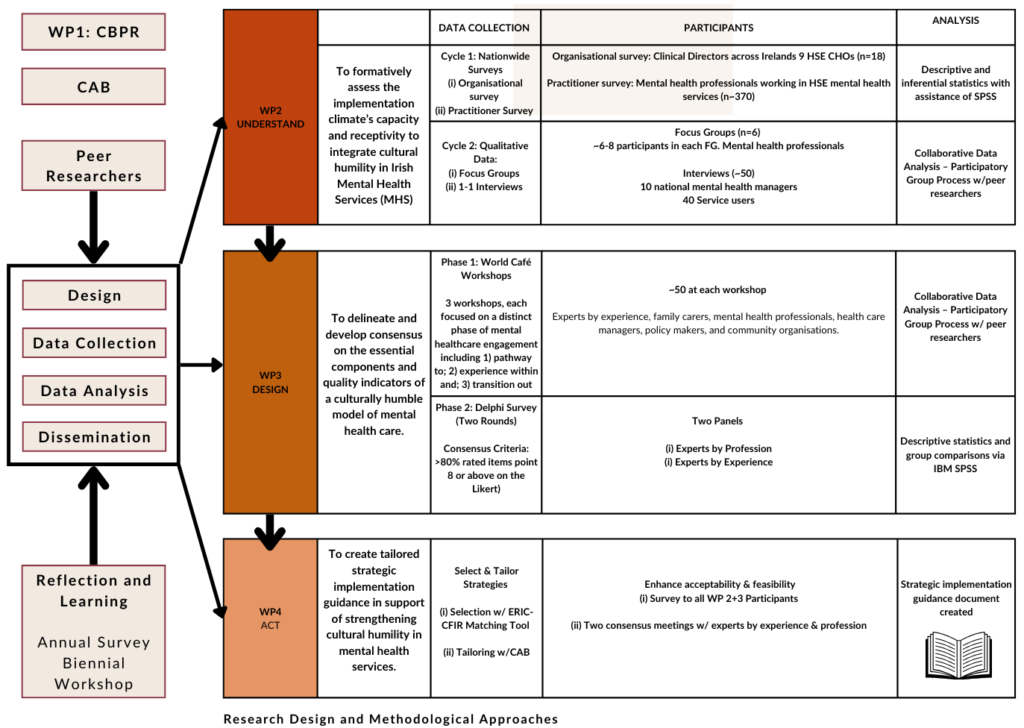
In The CHUMS Study, the Community Advisory Board (CAB) plays a central role in integrating authentic Community-Based Participatory Research (CBPR) practices into the governance and conduct of the research program. The CAB is composed of a diverse group, including the academic research team, peer researchers, mental health practitioners, HSE managers, policymakers, individuals with lived mental health experience from ethnic minority backgrounds, and representatives from community organisations. Together, these members bring invaluable expertise and “information power,” enabling them to guide and continuously refine the CBPR process by iteratively reflecting on and enhancing the study’s approach across its entire lifespan.







Impact
The CHUMS Study aims to make a lasting impact on mental health services in Ireland by advancing culturally humble care practices. Through our findings, we will provide evidence and practical recommendations to help mental health services adopt and integrate a culturally responsive model of mental health care tailored to the needs of ethnic minority communities. We envision that The CHUMS Study will foster a more inclusive and supportive environment for both practitioners and service users, ultimately enhancing the quality and accessibility of care for everyone. The CHUMS Study team are focused on ensuring the knowledge generated will be implementable within our current mental health services. In support of reducing the research to practice gap, we will co-design a strategic implementation blueprint to guide the effective implementation of cultural humility in mental health services.
The CHUMS Study Team

Dr Becca Murphy
Assistant Professor in Mental Health, DCU School of Nursing, Psychotherapy, and Community Health
Dr Becca Murphy, the principal investigator of The CHUMS Study, is a sociologist with expertise in participatory qualitative methodologies and implementation science within the field of mental health systems. Her work focuses on amplifying and integrating the knowledge of Experts by Experience in both our mental health and research systems and has extensive experience of conducting participatory methodologies with normatively excluded and ‘minoritised’ communities. Her work is also informed by implementation science, specifically the co-design, implementation, and scaling of ‘optimised’ interventions in mental health systems.

Yukti Arora
Yukti Arora is the Research Assistant on the CHUMS Study. She holds a Master’s degree in Counselling Psychology from India and has worked as a Psychological First Aid provider at Tihar Prisons, one of Asia’s largest correctional facilities. She has also collaborated with a non-profit organisation in India before moving to Ireland, engaging with vulnerable populations and contributing to their programs. Her research interests focus on looking at mental health and trauma through a cross-cultural lens and working with ethnic minority populations. Yukti recently completed her MPhil in Psychoanalytic Studies from Trinity College Dublin, where she deepened her understanding of psychoanalytic theory and its application to diverse mental health experiences.

Dr Zahra Farahani
Dr Zahra Farahani is the research fellow working on the CHUMS Study. Before joining DCU, Zahra was a postdoctoral researcher at the UCD School of Psychology working on the 3SET project on student mental health services. She completed her PhD at UCD School of Psychology on the experience of inclusion of Muslim migrant women and their children in Ireland and her master’s degree in clinical psychology in her home country, Iran. Zahra’s research is focused on mental health, wellbeing, and inclusion of ethnic minoritised, migrants and the youth population with a specific interest in the development, evaluation, and improvement of mental health services.

Ethel Matarutse
Ethel Matarutse is a PhD student in the School of Nursing, Psychotherapy, and Community Health, working under the supervision of Dr Rebecca Murphy and Professor Dawn Edge. Ethel completed her BSc (Hons) degree in Psychiatric Nursing at Dundalk Institute of Technology and recently graduated from DCU with an MSc in Health and Social Inclusion Program. Her MSc research explored how mental healthcare providers understand and address the religious/spiritual beliefs of Black and Minority Ethnic service users in Ireland, and she is exploring it further in her PhD within the context of The CHUMS Study. Ethel is a Registered Psychiatric Nurse and has gained clinical experience having recently worked as a staff nurse with the HSE in an acute mental health hospital. Her research interests include mental health, religion/spirituality, and culture in mental health, understanding the meanings, expressions and explanations of mental health and mental illness of ethnic minorities.
Our Peer Researchers

Julie Duke Mc-Donagh
Julie Duke-McDonagh is a proud Irish Traveller and a qualified peer support worker in mental health, currently working part-time with the HSE. Drawing from her own lived experience with mental health challenges, Julie is a passionate advocate for raising awareness, reducing stigma, and encouraging open conversations about mental health, particularly within the Traveller community. Julie delivers talks at colleges, conferences, and mental health teams, sharing her insights and experiences to inspire change. She is also a peer researcher on the Strengthening Cultural Humility in Irish Mental Health Services project. Her work focuses on fostering small but meaningful changes within her community, aiming to show the benefits of seeking support and addressing mental health needs openly.

William Lawrence
William is a dedicated mental health worker passionate about supporting his community through his role at Exchange House Ireland National Traveller Service. As a Traveller man, he provides peer support to Traveller men in prison and their families, offering guidance and encouragement during challenging times. He has also led a Traveller Support Group at Mountjoy Prison, fostering connection and resilience among participants. A certified SafeTALK Trainer, William empowers others to recognise and respond to signs of suicidal behaviour. His work reflects a deep commitment to creating positive, lasting change within the Traveller community and beyond.
Our Academic Partners

Prof. Dawn Edge
Prof. Dawn Edge is a Professor of Mental Health & Inclusivity in the Division of Psychology & Mental Health at the School of Health Sciences, University of Manchester. As the University's Academic Lead for Equality, Diversity & Inclusion (ED&I), Prof. Edge provides leadership and support to advance ED&I objectives across faculties, schools, and professional services and supports initiatives such as the Athena SWAN and Race Equality Charter. Committed to integrating research, policy, and practice, Prof. Edge works closely with communities to improve health and wellbeing, particularly for marginalized and socially excluded groups.

Dr Frédérique Vallières
Dr. Vallières is an Associate Professor in Global Health at Trinity College Dublin (Ireland) and Director of the Trinity Centre for Global Health. Her research prioritises the use of participatory approaches to study individual, community, and system-level responses to catastrophic life events so as to better understand how mental health services and systems can better respond to - and recover from – potentially traumatic events.

Dr. Pat Bracken
Dr. Pat Bracken is a consultant psychiatrist and philosopher with extensive experience in the fields of global mental health, post-traumatic stress, and critical psychiatry. He has held leadership roles, including Clinical Director of Mental Health Services in West Cork, Ireland, and continues to work at the intersection of psychiatry, ethics, and social justice. Dr. Bracken is known for his focus on person-centered and community-based approaches to mental health care, challenging traditional frameworks, and advocating for compassionate, collaborative practices. He is a co-founder of the Critical Psychiatry Network and has contributed to shaping mental health care globally through his research, teaching, and policy work.

Prof. Kwame McKenzie
Dr. Kwame McKenzie is a Senior Scientist at the Institute for Mental Health Policy Research and Director of Health Equity at the Centre for Addiction and Mental Health (CAMH). He serves as a full professor and Co-Director of the Division of Equity, Gender, and Population in the Department of Psychiatry at the University of Toronto. Dr. McKenzie is also the CEO of the Wellesley Institute and a member of the Mental Health and Addictions Advisory Council to the Minister of Health. An international expert on the social causes of mental illness, suicide, and equitable health systems, Dr. McKenzie has over two decades of experience in cross-cultural health research. Alongside his research and policy work, Dr. McKenzie continues to see patients, train clinicians, and contribute to international health initiatives.

Dr. Byron Powell
Byron Powell is an Associate Professor and Associate Dean for Research at the Brown School at Washington University in St. Louis. He is the Co-Director of the Brown School’s Center for Mental Health Services Research; Co-Director of the Institute for Public Health’s Center for Dissemination & Implementation, for which he leads the Implementation Methods & Metascience Initiative; and Co-Director of the Institute of Clinical and Translational Science’s Dissemination and Implementation Research Core. Byron is a Past President of the Society for Implementation Research Collaboration, Co-Editor-in-Chief of Implementation Research and Practice, and he serves on the editorial board of Implementation Science.

Dr. Jon Salsberg
Jon is an associate professor of primary healthcare research – public and patient involvement, and UL site lead for the PPI Ignite Network. He is a public health researcher with a background in health promotion and the anthropology of development. His research interests are in understanding the theory and practice of multi-stakeholder engagement for co-creating new knowledge and its translation into action in primary health care and community health. Jon has undertaken partnered research involving a broad range of stakeholders including patients, health practitioners, community organisations, policymakers and health service decision-makers, and has worked extensively with Indigenous communities, particularly the award-winning Kahnawake Schools Diabetes Prevention Project (KSDPP).
Our Community Partners








