TS4TIC: Translational Simulation for
Trauma Informed Care
Co-developing, piloting and evaluating a translational simulation delivery model for the promotion of psychological trauma-informed care to improve service delivery within acute hospital settings
BACKGROUND
Psychological trauma results from exposure to a single event or a series of events that are experienced as emotionally or physically harmful. Single traumatic events (i.e., an accident, house fire or assault), or repeat traumatic events (i.e., childhood abuse, domestic violence, war, homelessness, poverty, mental health conditions, racism, or ableism) can all result in psychological trauma that may lead to life-altering consequences. Psychological trauma may overwhelm a person’s coping capacity and perpetuate detrimental long-term effects on physical and mental health and well-being. As 70% of the adult population report experiences of psychological trauma (Benjet, et. al., 2016), it is highly likely that hospital staff encounter patients with psychological trauma histories every day, with challenging interactions between patients and staff that place patients at increased risk of avoidable patient safety events and poorer health outcomes. Recognising the prevalence and potentially injurious effects of psychological trauma among healthcare workers and patients alike is considered important to ensure patient engagement, quality of care, positive health outcomes, as well as improved staff wellness, and more resilient health systems.
OUR APPROACH
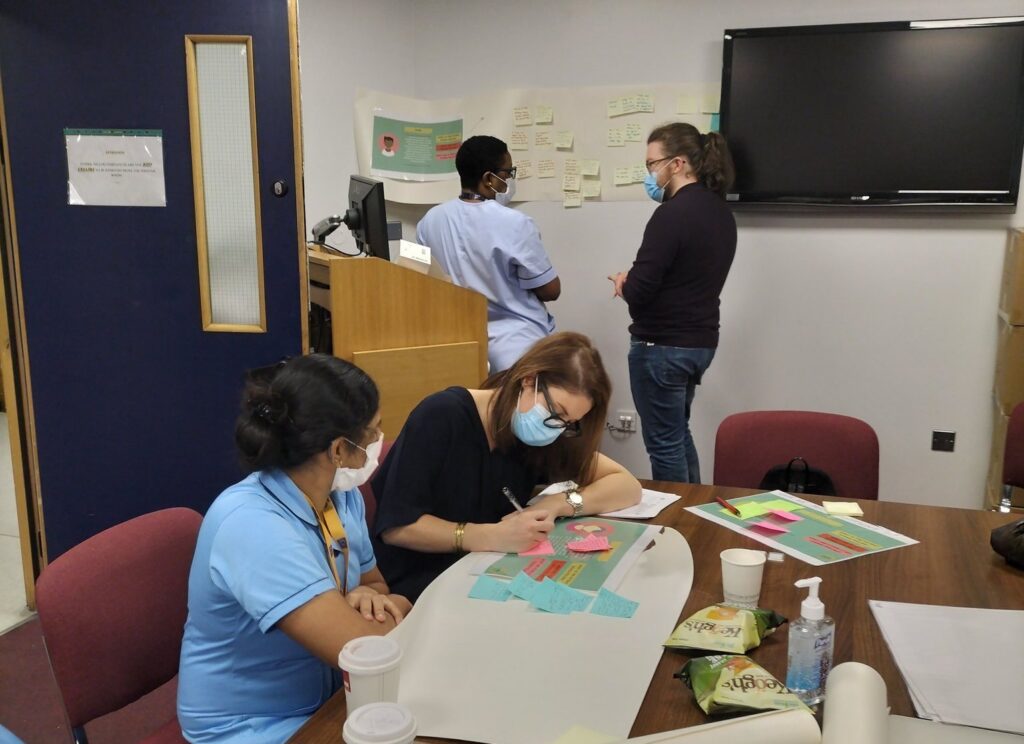
Underpinning the Institute for Healthcare Improvement (IHI) Model for Improvement, we are using the novel approach of translational simulation (TS), a simulation methodology that aims to improve patient care and health systems. It uses a team-based, in-situ simulation of challenging scenarios to improve patient care and healthcare systems. The focus of TS in this project is on team behaviours and systems-level learning and change rather than on individual knowledge. Using TS approaches, we are currently co-designing and implementing a trauma-informed care (TIC) improvement programme for use in acute hospital settings.
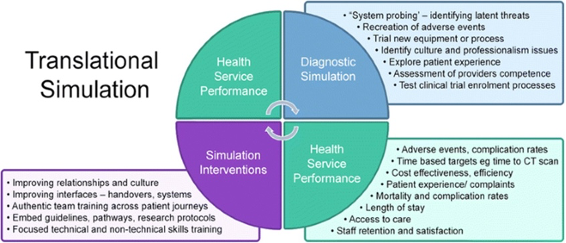
Stages of implementing translational simulation have been reproduced with permission from Brazil, V. (2017)
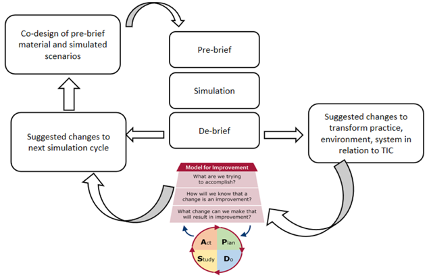
Adapted from the Institute for Health Improvement (IHI) model for improvement
The co-development and subsequent evaluation of the programme is being achieved using a mixed-methods, collaborative approach through a combination of TS with the IHI Model for Improvement and Demming’s PDSA cycles. This process entails the co-development of translational simulation for trauma-informed care (TS4TIC) improvement programme [Plan], carrying out the TS4TIC training and improvements [Do], observing and learning from the processes and outcomes of TS4TIC [Study], and determining what modifications are to be made in the next iteration of the TS4TIC improvement programme [Act].
The TS scenarios have been developed with input from service user representatives and staff. Debrief sessions following simulations are also being conducted which provide an opportunity to explore learning and focus on the use of trauma-informed skills such as establishing trust, offering choice, empowering patients, active listening, showing cultural sensitivity, improving trauma awareness, as well as seeking guidance from staff on how the hospital could support more of the use of these skills in frontline practice. Six simulations have been completed to date, with 42 participants from catering, healthcare assistance, nursing, occupational therapy, physiotherapy and security taking part. Staff from all areas are encouraged to take part. The simulations have received appreciation through positive feedback from participants.
References:
- Benjet C, Bromet E, Karam EG, et al.: The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychol Med. 2016; 46(2): 327–343.
- Brazil V: Translational simulation: Not ‘where?’ but ‘why?’ A functional view of in situ simulation. Adv Simul (Lond). 2017; 2(1): 20.



IMPACT
An open-access TS4TIC Toolkit has been developed that provides guidance on how to use a form of healthcare simulation, transformative simulation, to introduce or explore the principles of trauma-informed care with healthcare staff. The toolkit supports healthcare organisations to use simulation to improve patient experiences and deliver quality improvements in the wider system. The toolkit is targeted at acute or community healthcare organisations of any size who are interested in using TS as a methodology to explore the principles of TIC.
We envision that the below resources will considerably impact the work environment for healthcare workers, along with improving quality of care and patient experiences among all those accessing services. Apart from this, we foresee an impact on curriculum development within our partner academic teaching hospitals, while also impacting existing methods and theory, towards the advancement of new approaches to achieve system change.
You can access the study protocol here or refer to the below project resources.
OUR TEAM
We are a group of people consisting of: people with lived experiences of psychological trauma; front-line and executive hospital staff including doctors, nurses, security staff and other health and social care professionals; and researchers with extensive experience in psychological trauma. Together, we understand first-hand the impact that psychological trauma has in healthcare settings, the effects of which have been worsened by the COVID-19 pandemic.

Dr Frédérique Vallières
Associate Professor, Global Health and Psychology, and Director, Trinity Centre for Global HealthDr Vallières’ (BSc, MSc, PhD) current research focuses on the application of Psychology to Global Health, with a focus on Global Mental Health, Health System Strengthening, and Human Resources for Health. Concerned with closing the research-to-practice gap prevalent within Global Health, Dr. Vallières prioritises working in close collaboration with civil society organisations and through multidisciplinary consortiums comprising European, sub-Saharan African, Asian, and Middle Eastern partners. As Dr. Clíona Ní Cheallaigh’s co-PI, Dr. Vallières is responsible for the research component of TS4TIC.

Sinead Murray
Project LeadSinead is a social worker with practice and management experience in acute hospital settings. She is a Member of the Board of the Irish Association of Social Workers, with a special interest in advocacy in upholding rights, addressing inequalities, safeguarding & disability.

Dr Marie Ward
Health Systems Learning and Research Facilitator, Quality and Safety Improvement Directorate, St James’s HospitalDr Ward is an embedded researcher at St James’s Hospital Dublin, Ireland where she is engaged in a programme of Health Systems Research and Improvement. Marie holds a PhD in Psychology Human Factors from TCD and is an Adjunct Assistant Professor at TCD’s multidisciplinary Centre for Innovative Human Systems. Marie is a lecturer on the Masters in Managing Risk and System Change (TCD) and the Masters in Human Factors in Patient Safety at the RCSI; Chairperson of the Irish Human Factors and Ergonomics Society. Her research interests include how to enable patient and staff safety and wellbeing from a systems perspective and co-designing new systems from a socio-technical perspective.

Dr Meg Ryan
Assistant Professor, Trinity Centre for Global HealthDr Ryan is an Assistant Professor in Global Health with the Trinity Centre for Global Health, and a Chartered Counselling Psychologist. She is a research collaborator on the TS4TIC project, assisting with data collection and analysis and the co-development of the translational simulation scenarios.

Mel Swords
Research Assistant, Trinity Centre for Global HealthMel is an MSc in Applied Psychology graduate and research assistant on TS4TIC. He is currently managing the KTA award which seeks to develop trauma-informed teaching aids for third-level health undergraduates, for use by their educators to introduce them to the principles of trauma-informed care.

Dr Clíona Ní Cheallaigh
Associate Professor, Department of Clinical Medicine, Trinity College Dublin, and Consultant, Infectious Diseases and General Medicine in St James’s HospitalDr Cheallaigh is the co-PI on this project and the Clinical Lead of the Inclusion Health Service in St James’s Hospital dedicated to improving access to specialist hospital care for socially excluded individuals. Her research seeks to look at the effect of social exclusion on health from a number of perspectives, and includes work on health systems design and evaluation, work funded by the HRB on premature ageing in homeless adults and work on the effect of social exclusion on the immune system funded by the Royal City of Dublin Hospitals Trust.

Prof Una Geary
Consultant in Emergency Medicine and Director for Quality and Safety Improvement, St James’s HospitalProf Geary is a graduate of the University of Dublin, Trinity College. She completed basic specialty training in general internal medicine in Dublin and went on to undertake higher specialist training in Emergency Medicine in the UK. She also worked in Australia and the USA during her Emergency Medicine training. She was a Consultant in Emergency Medicine at the Royal Liverpool University Hospital Trust, UK, for five years before returning to St James’s Hospital in 2003. Prof. Geary was Clinical Lead for the National Emergency Medicine Programme from 2010 to 2013. She completed the Diploma in Quality and Leadership at the RCPI and the Masters in Managing Risk and System Change at TCD. Prof. Geary is a member of the National Independent Patient Safety Council and a former Board Member of HIQA.

Dr Darragh Shields
Emergency Medicine Consultant and Director of Medical Education, St James’s HospitalDr Shields is an Emergency Medicine Consultant in St James’s Hospital and is the Director of Medical Education at St James’s Hospital. He holds an MSc in Healthcare Simulation and Patient Safety from the College of Medicine, Nursing, & Health Sciences, School of Medicine, NUIG and in Health Professionals Education from the Royal, College of Surgeons Ireland. He is a member of the Project Steering Committee.

Dr Becca Murphy
Assistant Professor, Social Science in DCU School of Nursing, Psychotherapy, and Community Health and Programme Chair, MSc in Health and Social InclusionDr Murphy is a sociologist with expertise in participatory qualitative methodologies and implementation science within the field of mental health systems. Her work focuses on amplifying and integrating the knowledge of Experts by Experience in both our mental health and research systems and has extensive experience of conducting participatory methodologies with normatively excluded and ‘minoritised’ communities. Her work is also informed by implementation science, specifically the co-design, implementation, and scaling of ‘optimised’ interventions in mental health systems.
OUR PARTNERS